Early in the COVID-19 pandemic, the guidance on non-pharmaceutical interventions was much different from that in place today. Initially, mask use was not supported by many Western government agencies, with the US Surgeon General explaining (in a now deleted tweet posted on 29 February 2020): ‘Seriously People – STOP BUYING MASKS! They are NOT effective …’
The World Health Organization was also in on the action, releasing a scientific brief on 29 March 2020 emphasising that COVID-19 was not airborne (bit.ly/3BeiC58).
While recommendations have clearly changed since then, it took fresh data (bit.ly/3nt8hgF) to overcome old beliefs on viral transmission. In the process, it has fundamentally changed how we view respiratory viruses.
Aerosol scientists take a stand
Not everyone was on board with initial guidance that downplayed the potential for airborne transmission of COVID-19, to put it lightly. Many aerosol chemists did not feel that the WHO was actively listening to their concerns regarding the need for a more cautious approach to public health guidelines.
One of the most vocal critics was Professor Donald Milton at the School of Public Health, University of Maryland, USA, whose reply to the WHO regarding their rejection of aerosol transmission left no room for misinterpretation: ‘I think the WHO is being irresponsible in giving out that information. This misinformation is dangerous’ (n.pr/3GiSWbj).
It’s not often the WHO gets called out for misinformation by a world-leading scientist. But that’s exactly what happened in April 2020. And Milton wasn’t alone. In July 2020, Milton and QUT physicist and aerosol researcher Lidia Morawska published an open letter that was co-signed by 239 experts in the field, calling for the international medical community to recognise the threat of aerosol transmission (also referred to as airborne transmission) (bit.ly/3mlBpY5).
Aerosol assumptions
One particular focus of aerosol researchers was the restrictive limits that medical officials put on aerosol travel, which were the basis for the recommendations on social distancing. The idea that respiratory particles could only travel 2 metres was based on historical assumptions, not recent data. In fact, it went against the very physics that defined the field of aerosol science.
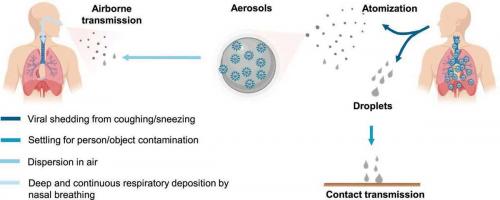
In the early guidance on COVID-19 transmission, there was a distinct cut-off size (5 μm) for defining respiratory particles. Anything smaller than 5 μm was considered by health officials as an aerosol and anything larger than 5 μm was labelled as a droplet. The prevailing opinion among the medical community was that droplets greater than 5 μm were large enough to succumb to the forces of gravity, falling to the ground within 2 metres of being expelled.
This assumption was not in line with aerosol scientists’ understanding of how airborne particles behave. The transport and fate of aerosol particles depends on their size, and particles larger than 5 μm can travel much farther than 2 metres under normal conditions. In a room with stagnant air flow, aerosols can travel around 10 metres and remain airborne for hours. The more appropriate threshold used by aerosol scientists is 100 µm, the size that better separates particles on their aerodynamic behaviour. Thus, to aerosol scientists, anything smaller than 100 µm (rather than 5 μm) is defined as an aerosol, as these sizes can remain suspended in the air for more than 5 seconds when released from a height of 1.5 metres.
The disagreement in terminology highlighted the disconnect between aerosol researchers and public health officials. Particles larger than 5 μm are regularly exhaled in breath, yet public health protocols were based on the assumption that exposure to these respiratory particles could be easily mitigated by social distancing. Furthermore, the smaller aerosol particles less than 5 μm were being overlooked, yet they were actually the most important with regard to transmission.
Respiratory particle generation
When someone coughs, talks or even breathes, most of the particles released are of the smaller variety rather than the larger droplets, with particle concentrations on the order of thousands per litre of air. These aerosol particles are also the ones most likely to transmit SARS-CoV-2, as viruses are typically enriched in respiratory particles smaller than 5 µm.
The asymmetric viral distribution within particle sizes relates to how respiratory aerosols are generated. During breathing, the smaller aerosol particles are created when air interacts with the thin liquid film lining the respiratory tract. Conversely, the larger particles are primarily created by air passing through the oral cavity and interacting with saliva. As airflow and speech volume increase during activities such as singing and shouting, greater numbers of aerosols are produced.
The small size of virus-laden aerosol particles also affects their ability to cause infection. The smaller the particle, the deeper it can penetrate the respiratory system when inhaled. Thus, the smallest particles – those less than 5 μm – can deposit in the lungs, causing lower respiratory infection and potentially requiring smaller viral concentrations to do so than intranasal and upper airway infections.
Evolution of aerosol data
When considering guidelines and health recommendations, the WHO traditionally requires a high evidentiary threshold for implementing changes. While this ensures the organisation consistently reports well-established scientific opinions, it also means that an outdated disposition is harder to correct. To redefine aerosol transmission related to COVID-19, the WHO desired more robust studies and a higher burden of proof. However, investigating viral transmission, especially via tiny aerosol particles, is no easy task in a laboratory environment. Besides the technical challenges associated with measuring RNA concentrations in particles smaller than 5 μm in diameter, attempting to determine the amount of viral RNA required to initiate infection also remains difficult.
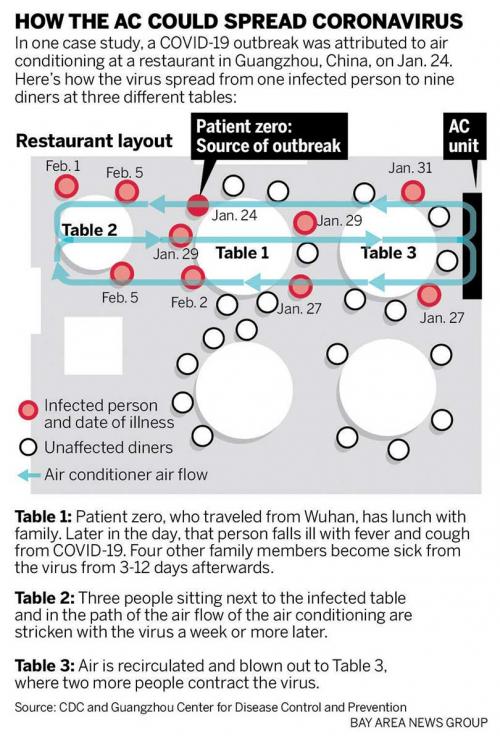
As the pandemic progressed, epidemiological studies were able to highlight the prevalence of aerosol transmission. At a restaurant in Guangzhou (China) in January 2020, nine patrons sitting within the airflow of a single asymptomatic case became infected despite no close interactions (bit.ly/3jCfr0U). In February 2020, reports from the Diamond Princess cruise ship quarantined at a Japanese port suggested that passengers may have been infected via long-range transport, an assertion that was supported by later modelling work (bit.ly/3jCfycQ). The next month, a superspreading event occurred during a church choir rehearsal in the USA where 53 of the 61 members became infected despite following social distancing protocols (bit.ly/2XJ7hw0). In Australia, long-range transmission at a Western Sydney church service occurred in July 2020, leading to 12 secondary cases, including one that was 15 metres away from the index case. Further events at meat packaging plants (bit.ly/3pAfWwf), across hotel hallways in New Zealand, and from rows apart during air travel (bit.ly/3vOenfh) supported the airborne nature of the virus.
By April 2021, the WHO had declared that aerosols were the dominant mode of transmission for COVID-19, nearly a year after aerosol chemists had come to the same conclusion (bit.ly/3jWevF5). With airborne respiratory particles now at the forefront of the COVID-19 pandemic, updated public safety protocols and recommendations have been needed to reflect the newly gained knowledge.
Ventilation, masks and distancing
Perhaps the most important change in the future is to apply better indoor ventilation strategies. Nearly all superspreader events have happened in indoor environments where airflow is reduced compared with outdoor areas. Since aerosols can concentrate indoors, a greater emphasis on clean air exchange is required inside areas of habitation. In buildings with central air, greater outdoor air exchange can be used alongside higher efficiency filters, with current advice recommending filters with a minimum efficiency reporting value of at least 13. Stand-alone HEPA (high-efficiency particulate air) filters can also be used to help clean re-circulated air, and there is potential for using upper room UV treatment to deactivate viruses.
In the absence of a central air system, the simple act of opening a window can improve ventilation by up to a factor of three. Current recommendations state that, ideally, indoor environments should have at least four to six air changes per hour. The use of carbon dioxide sensors could also be of use when trying to monitor the amount of exhaled breath in certain indoor environments, with target concentrations below 800–1000 ppm CO2 recommended. Cleaner indoor air would have long-ranging benefits beyond viral infections, as polluted indoor environments are associated with increased incidences of respiratory illness and decreased cognitive performance.
In addition to ventilation, proper mask use can help reduce COVID-19 transmission. Health guidelines were originally updated to recommend mask use when it was discovered that asymptomatic and pre-symptomatic individuals could transmit the virus. Now, the most effective types of masks and their fit also should be added to recommendations. Single-layer cloth masks, like scarves and bandanas, are far less useful than triple-layer cloth masks, surgical masks and N95 respirators. N95 masks, which can filter at least 95% of particles, have the best filtration efficiency if worn correctly, although the limited supply and fit testing required for their optimal use make them less practical in many applications. Surgical masks are typically 50–75% efficient; however, their efficiency can be improved to 60–90% by modifying the fit for a better seal around the face or by using them in combination with a tightly fitted cloth mask. Overall, even if a mask is not completely effective, widespread use across a community can help reduce viral transmission.
A better understanding of the social distancing guidelines could be beneficial as well. While virus-laden aerosols can infect at any nearby distance, the large droplets theoretically would be relevant to the 2 metres closest to another individual, regardless of indoor or outdoor location. Distancing within indoor environments should be as far as allowable. Much like with other interventions, a 2-metre distance doesn’t guarantee safety from the virus, and it is best to use a combination of preventative approaches to help lower the spread of COVID-19.
With the insight gained from COVID-19 research, experts now have more confidence that other respiratory viruses have similar airborne properties, such as influenza, respiratory syncytial virus and human rhinovirus. Thus, the interventions we apply to help fight COVID-19 are likely to help keep communities safe beyond the realm of the current pandemic.